We are proudly partnered with OptumRx. They have a team of pharmacists, care management and customer service advocates all working to make sure you get the medication you need, conveniently and cost-effectively.
The Fund Office also has a Pharmacy Benefit Department that works as a liaison between the membership and OptumRx.
The Prescription Drug Program provides eligible retired members of Local 150, and their eligible dependents who are eligible for Medicare, benefits through the Midwest Operating Engineers Retiree Welfare Plan Medicare Prescription Drug Plan (RWP Medicare PDP).
The RWP Medicare PDP combines a standard Medicare Part D prescription drug plan with additional coverage provided by the RWP. This additional coverage is also referred to as a wrap plan because it wraps around the standard Medicare Part D plan and closes the gaps between Part D and your pre-Medicare coverage from the Prescription Drug Program. This means that you will have more coverage than the standard Medicare Part D plan.
Under RWP Medicare PDP you can:
- Fill your medication for a 30 or 90-day supply
- Always fill your medication at any in-network pharmacy (you are not required to fill maintenance medications at CVS)
This additional coverage is also referred to as a wrap plan because it wraps around the standard Medicare Part D plan and closes the gaps between Medicare Part D and your pre-Medicare coverage you had under the Prescription Drug Program. The wrap plan covers prescription drugs not normally covered under Medicare Part D, such as medications used for anorexia, weight loss or weight gain, medications used for the symptomatic relief of cough or cold, prescription vitamins and mineral products not covered by Part D, and medications used for the treatment of sexual or erectile dysfunction.
The Plan allows you to fill a 30-day supply or up to a 90-day supply of prescription medication at any OptumRx network pharmacy or the Optum Home Delivery pharmacy. Just be sure to present your OptumRx MedicareRx ID card at your network pharmacy so your prescriptions are accurately billed.
To find a list of the OptumRx network pharmacies, you can visit the OptumRx website at optumrx.com and use the “Pharmacy Locator” tool (found under the “Member Tools” tab). You can also call OptumRx Member Services at 866-868-2493 for help or to request a copy of the list to be mailed to you.
The RWP Medicare PDP copay structure is outlined in the chart below.
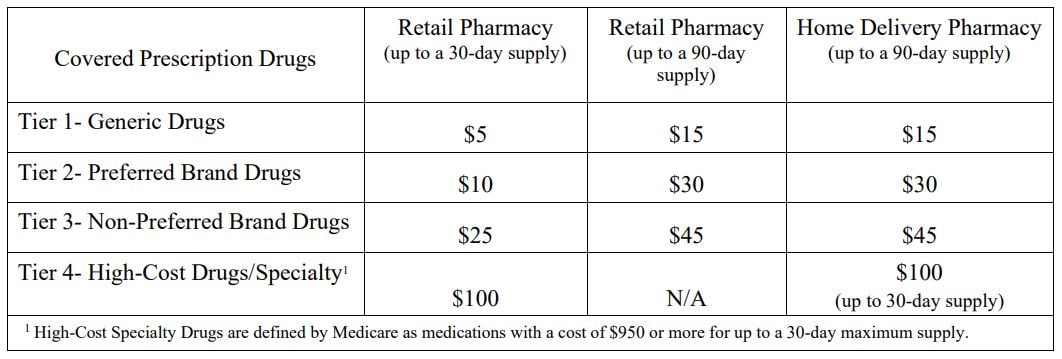
For Medicare-eligible Retirees, we follow the RWP Medicare PDP formulary (linked at top of page). This is a guide within select therapeutic categories for Plan members and health care providers. Ask your physician to consider prescribing generic medication as a first line option, when medically appropriate. Generic medications are typically a lower cost to the plan, and these savings are immediately passed directly to the membership. If there is no generic available, there may be a preferred brand name medication listed.
If you pay out-of-pocket for a prescription, you have to file a claim with OptumRx for reimbursement. The Fund Office does not process RWP Medicare PDP out-of-pocket reimbursement requests.
For consideration of reimbursement, complete a Medicare Part D Claim form and mail the form along with your register receipts to:
OptumRx Claims Department
P.O. Box 650287
Dallas, TX 75265
If the claim is not approved, there will be no reimbursement. If the claim is approved, you will be reimbursed the amount you paid minus your copayment.
If your prescription is rejecting due to a PA required, the pharmacy should reach out to your physician. In the event that your physician does not receive this information from the pharmacy or you would like to expedite the PA process, we recommend that you follow up with your physician’s office.
Your physician can initiate a PA with OptumRx by doing any of the following:
- Call the OptumRx PA department at (800) 711-4555
- Electronic (ePA):https://www.covermymeds.com/epa/optumrx/
All PA’s are reviewed by clinicians at OptumRx, not the Pharmacy Benefit Department at the Fund Office.
If you would like to check on the status of your PA, contact OptumRx Member Services at (866) 868-2493.
Specialty medications require a prior authorization before they can be filled. To determine if your specialty/high-cost medication is covered, contact OptumRx Member Services at (866) 868-2493.
You can fill your specialty/high-cost medication at any network specialty pharmacy listed on your OptumRx Pharmacy Directory. The Pharmacy Directory is mailed by OptumRx annually and contains the pharmacies in your area within a 20-mile radius based on your zip code. If you need to locate a specialty pharmacy and you do not have access to your Pharmacy Directory, contact OptumRx Member Services at (866) 868-2493.
Yes, but certain requirements have to be met for it to be covered by the RWP Medicare PDP. For more information, contact OptumRx Member Services at (866) 868-2493.
Yes. For a list of covered vaccines refer to the RWP Medicare PDP formulary linked at top of page. RWP Medicare PDP covered vaccines are $0 if obtained at a network pharmacy.